Education
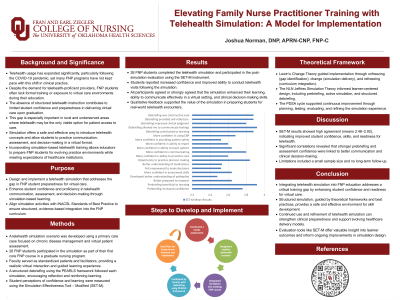
(67) Elevating Family Nurse Practitioner Training with Telehealth Simulation: A Model for Implementation
Thursday, June 19, 2025
5:00 PM - 6:30 PM MST
Location: Exhibit Hall
Joshua D. Norman, DNP, APRN-CNP, FNP-C (he/him/his)
Clinical Assistant Professor
University of Oklahoma Fran and Earl Ziegler College of Nursing
Oklahoma City, Oklahoma, United States
Lead Author(s)
Abstract: To address limited telehealth training in Family Nurse Practitioner (FNP) programs, this project implemented a telehealth simulation to enhance FNP students’ practical skills and confidence. Utilizing Lewin’s Change Theory for guided implementation and NLN Jeffries Simulation Theory for educational design, the simulation integrated realistic patient communication, assessment, and care planning in a virtual primary care scenario.
The simulation was conducted with 26 FNP students in their first core course at a college of nursing in Oklahoma. Faculty members acted as standardized patients, ensuring authenticity in learner-patient interactions. Debriefing followed the PEARLS framework, allowing reflective learning and feedback to reinforce key telehealth skills.
Evaluation via the Simulation Effectiveness Tool – Modified (SET-M) measured student outcomes in self-assessed confidence and competence, showing significant increases across all telehealth competencies. The SET-M, a validated tool with high reliability, provided structured insight into student learning.
This project illustrates how structured telehealth simulations in FNP curricula can effectively address training gaps. The findings support the effectiveness of structured telehealth simulations within FNP curricula, highlighting the potential for broader application to prepare students for the demands of virtual care. Integrating telehealth simulations into FNP education addresses current training gaps and aligns with advancing healthcare technology and simulation-based learning.
Please include a short summary of your presentation that highlights why an attendee would want to view your poster.: Explore how innovative telehealth simulations enhance FNP education, bridging key training gaps and building essential virtual care skills. This poster reveals a practical model, grounded in proven theories, that increases student confidence and telehealth proficiency. Ideal for educators seeking to elevate simulation in NP curricula and prepare practitioners for today’s healthcare demands.
The simulation was conducted with 26 FNP students in their first core course at a college of nursing in Oklahoma. Faculty members acted as standardized patients, ensuring authenticity in learner-patient interactions. Debriefing followed the PEARLS framework, allowing reflective learning and feedback to reinforce key telehealth skills.
Evaluation via the Simulation Effectiveness Tool – Modified (SET-M) measured student outcomes in self-assessed confidence and competence, showing significant increases across all telehealth competencies. The SET-M, a validated tool with high reliability, provided structured insight into student learning.
This project illustrates how structured telehealth simulations in FNP curricula can effectively address training gaps. The findings support the effectiveness of structured telehealth simulations within FNP curricula, highlighting the potential for broader application to prepare students for the demands of virtual care. Integrating telehealth simulations into FNP education addresses current training gaps and aligns with advancing healthcare technology and simulation-based learning.
Please include a short summary of your presentation that highlights why an attendee would want to view your poster.: Explore how innovative telehealth simulations enhance FNP education, bridging key training gaps and building essential virtual care skills. This poster reveals a practical model, grounded in proven theories, that increases student confidence and telehealth proficiency. Ideal for educators seeking to elevate simulation in NP curricula and prepare practitioners for today’s healthcare demands.
Learning Objectives:
- List the steps involved in creating and implementing a telehealth simulation for FNP students to improve their proficiency and confidence in telehealth practices.
- Identify key challenges and solutions in developing telehealth simulations specifically tailored for FNP education.
- Explain the impact of telehealth simulation on FNP student learning outcomes, including improved confidence and readiness for virtual patient care.
